What is the Pelvic Floor?
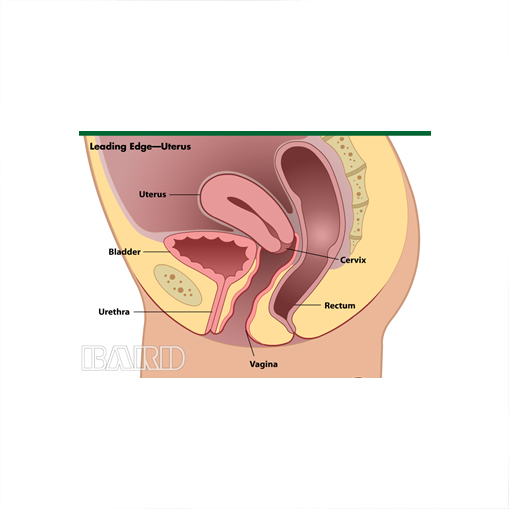
The pelvic floor is composed of muscles and ligaments that form a sling across the opening of the pelvis. Muscles and ligaments work together in the pelvis of women to support pelvic organs such as the vagina, uterus, urinary bladder and bowel. Pelvic floor disorders are caused by weakening support of the muscles, ligaments and connective tissue in the pelvis.
What is Pelvic Organ Prolapse?
Pelvic Organ Prolapse is the bulging or dropping of the uterus, rectum or bladder into the vagina. There are several different types of pelvic organ prolapse and it is common to have more than one type at the same time. While prolapse is not considered a life threatening condition, it may cause a great deal of discomfort and distress. The various types are:
- Cystocoele - when the bladder falls down into the vagina
- Uterine prolapse - when the womb drops down into the vagina
- Vaginal vault prolapse - when the vagina itself falls down
- Enterocoele - when the small bowel pushes against the vagina causing a bulge
- Rectocoele - when the rectal support becomes weak and bulges into the vagina
What is incontinence?
Incontinence occurs when women have trouble controlling their urine (urinary incontinence) or their bowels (fecal incontinence).
There are many possible causes of incontinence. The two most common forms of urinary incontinence are stress incontinence and urge incontinence. Others are Overflow incontinence and Mixed incontinence.
Stress incontinence happens when something you do – such as coughing, laughing, sneezing, jumping, lifting or exercising – increases the pressure in your abdomen enough that it pushes urine past the urethra. In other words, some external force pushes on the bladder and urine squirts out.
Urge incontinence happens when women are not able to wait until they empty their bladder. Women experiencing this problem say, that, "When I have to go, I have to go." This occurs because the normal ability of the nerves to give the message to the bladder to wait until it is the right time to pass urine is weakened. With urge incontinence, when a woman feels the need to empty her bladder, the message sent by the nerves to the bladder, to wait, simply doesn't work anymore. In this case either they have to immediately find a toilet or suffer from the extreme embarrassment of urinary leakage.
Overflow incontinence happens when the bladder gets overfilled and over flows. This can occur with medical conditions that desensitize the bladder sensory system. This may also occur when certain prolapses prevent complete emptying of the bladder.
Mixed Incontinence is a combination of one or more of the above.
What is urodynamic testing?
Urodynamic testing is a series of bladder tests that are done in order to observe how your lower urinary tract reacts under certain conditions. It is usually done to see if you have problems with loss of urine (urinary incontinence) or to figure out what type of incontinence you may have. Testing usually consists of filling your bladder with sterile water, then observing the pressure and how your bladder reacts under these increasing pressure conditions. When the test begins, the physician inserts a small soft catheter in your bladder and a tube is hooked up to a bag of sterile water. Your bladder is then filled to around 250 cc (approximately one cup), which most women can hold without needing to urinate. A second catheter, which is connected to a machine or computer, also is inserted. This catheter measures the pressures within your bladder. Once the bladder is filled, you will be asked to cough and strain in order to see how much urine you leak.
What is Interstitial Cystitis?
Interstitial Cystitis (IC) is a chronic condition of the bladder often causing symptoms of frequency, urgency, painful urination, painful intercourse and chronic pelvic pain. A common theory of Interstitial Cystitis is that it is a defect in the lining of the bladder (like an ulcer in the stomach). Treatment options include the bladder diet, medications, bladder lavage treatment and neuromodulation.
What treatment options are available for urinary incontinence?
Treatment options include habit training, prompted voiding, pelvic muscle rehabilitation (Kegel exercises), pessaries, medications and surgery.
Surgery is the only permanent treatment for prolapse and stress incontinence.
If I Do Nothing Will It Get Worse?
It may not happen quickly but, if left untreated, over time the condition often worsens. In rare instances, prolapse can cause urinary retention that may lead to kidney infection or permanent kidney damage. In these cases, treatment is necessary. Otherwise, the decision to treat the prolapse should be based on your signs and symptoms.
What is Anal Incontinence?
Anal incontinence is the involuntary leakage of gas, liquid stool or solid stool.
What causes Anal Incontinence?
Like other pelvic floor disorders, anal incontinence usually occurs because of childbirth. Even easy normal vaginal deliveries can result in direct injury to the anal sphincter muscle or to the innervations of the rectum and sphincter. About 15% of the time anal incontinence occurs because of direct injury to the anal sphincter. This may or may not be caused during childbirth. After childbirth you can often compensate for this problem. However as you grow older, the weakness of these muscles becomes more apparent. There are conditions that can lead to this disorder. Some of the more common ones include: Haemorrhoids or Haemorrhoid surgery, Radiation Enteritis, Spinal Cord Injuries, Inflammatory Bowel Disease, Multiple Sclerosis, Parkinson’s Disease, Stroke, Dementia, Diabetic Neuropathy, Rectal Prolapse and Descending Perineum Syndrome.
What Can Be Done To Treat Anal Incontinence?
There are different approaches to treating anal incontinence. The treatment depends upon the condition causing it. A complete history and physical examination will help identify the potential problems. Anal manometry, transanal ultrasound and pudendal nerve latency studies are diagnostic tests that are helpful in evaluation. Treatment options include dietary modifications, weight loss, bowel management, biofeedback, physical therapy and surgical options including anal sphincter repair, rectocele repair and sacral nerve neuromodulation.
When should I contact a doctor?
- If you have any concern at all about any condition with your body
- If you feel a bulge or lump inside or outside of your vagina
- If you have lower back pain or increased pelvic pressure that interferes with your daily activities
- If you have irregular vaginal spotting or bleeding
- If you experience frequent urinary incontinence, urinary tract infections, difficulty urinating, frequent urination or any of the symptoms listed here that interfere with your daily routine
- If you are experiencing any problems with your bowels mentioned above.
- If sexual intercourse is painful or difficult
How will I be evaluated?
When you see your doctor, you will have a detailed health history taken in order to get a thorough explanation of your symptoms. A pelvic examination is necessary to diagnose pelvic organ prolapse. If a prolapse is identified, your urogynaecologist will determine which organs are involved and the degree of the prolapse. Other test may be ordered based on the findings during history and examination.
Will treatment for prolapse affect my sex life?
If you choose to have surgery, you are asked to wait to have intercourse for a period of time (maximum 6 weeks), after which women report an improved sex life.
What can I expect at my first visit?
- The doctor will take a thorough history of your symptoms
- Pelvic examination
- Evaluation of pelvic support
- Evaluation of loss of urine or stool
- Neurological examination
- Evaluation of pelvic muscles
- Some blood tests
- You may be asked to fill a bladder diary and make follow up appointment
- Schedule surgery